Nursing
Ethical Dilemmas in Nursing: Strategies for Dealing


Navigating the complexities of modern healthcare places nurses at the crossroads of challenging ethical dilemmas. These situations demand not only clinical expertise but also a profound sense of moral responsibility. In nursing, ethical dilemmas arise when there are conflicting values, beliefs, and duties that make it difficult to determine the right course of action. This blog article delves into the realm of ethical dilemmas in nursing, exploring what they are, their significance, and the strategies for effectively managing them. From the perennial debate of pro-life vs. pro-choice to the sensitive intricacies of end-of-life care, patient confidentiality, and the allocation of scarce resources, we will examine common scenarios that nurses encounter. We will also discuss the balance between patient autonomy and medical advice, the impact of cultural and religious beliefs, and the ethical implications of using restraints.
Additionally, this article provides insights into handling unethical behavior by colleagues, disclosing medical errors, and practical approaches to dealing with these dilemmas. Join us as we unravel the ethical challenges in nursing and offer guidance on navigating these ethical dilemmas with compassion and integrity.
What are Ethical Dilemmas in Nursing
Ethical dilemmas in nursing arise when nurses face situations where they must choose between conflicting values, duties, or principles. These dilemmas often involve complex decisions that impact patient care and outcomes, such as balancing patient autonomy with medical advice or managing end-of-life care decisions. The nature of nursing, which requires close interaction with patients and their families, frequently brings nurses into contact with sensitive ethical issues. Navigating these dilemmas requires a deep understanding of ethical principles, compassion, and a commitment to patient well-being.

Need a Persuasive Essay on the Ethics of Patient Care?
Our writers are passionate about nursing and committed to delivering exceptional work.
Importance of Ethics in Nursing

The importance of ethics in nursing cannot be overstated, as it forms the foundation of patient care and professional integrity. Ethical principles guide nurses in making informed decisions that prioritize patient well-being, dignity, and rights. Upholding ethics in nursing ensures trust between patients and healthcare providers, fostering a safe and respectful environment. Additionally, a solid ethical framework helps nurses navigate complex situations, promoting accountability and high standards in the nursing profession.
Common Ethical Dilemmas in Nursing
Ethical dilemmas in nursing often challenge a nurse’s judgment and empathy, requiring careful consideration of various complex factors. Nurses frequently encounter challenging situations that test their professional and ethical standards. Here are some common ethical dilemmas in nursing:
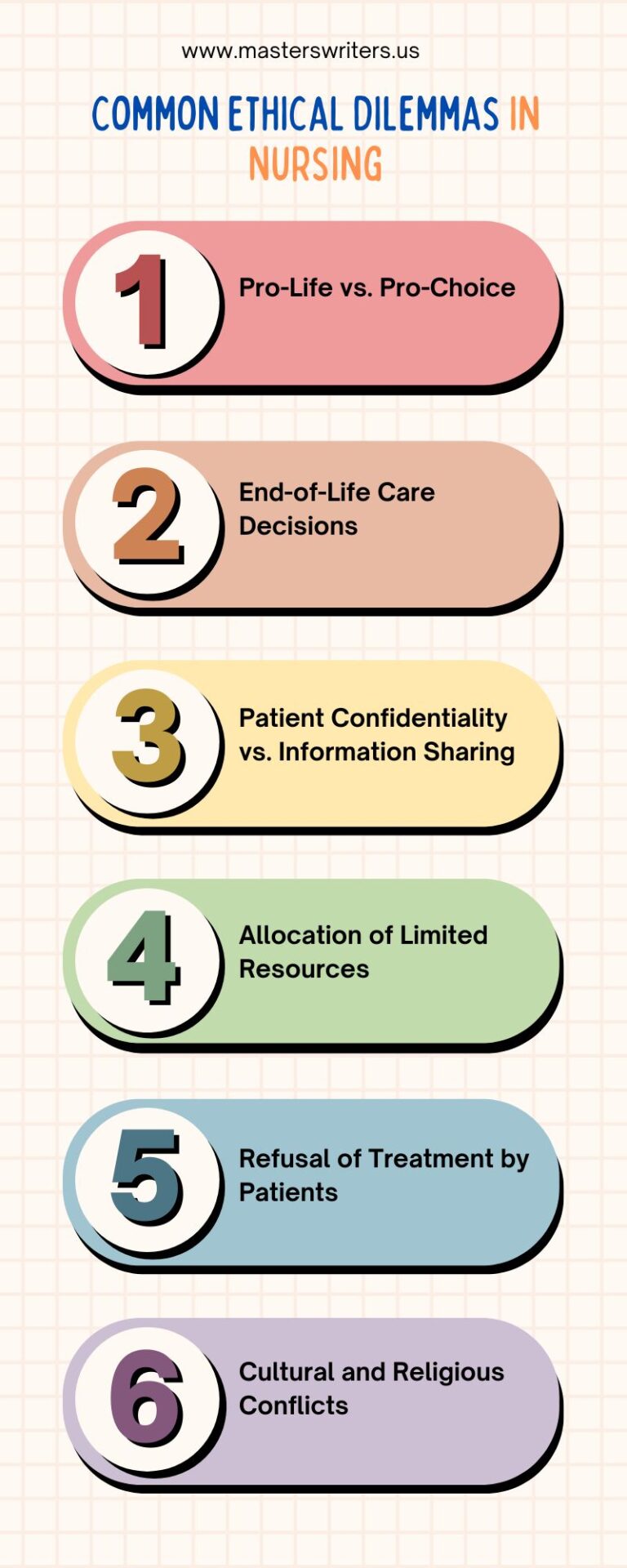
- Pro-Life vs. Pro-Choice
- End-of-Life Care Decisions
- Patient Confidentiality vs. Information Sharing
- Allocation of Limited Resources
- Refusal of Treatment by Patients
- Balancing Patient Autonomy with Medical Advice
- Cultural and Religious Conflicts
- Use of Restraints and Seclusion
- Handling Unethical Behavior by Colleagues
- Disclosing Medical Errors
Also, be sure to check out the essential steps for becoming a nurse practitioner that will get you started in this rewarding profession.
Pro-Life vs Pro-Choice
The debate over abortion is a deeply personal and controversial issue, creating significant ethical challenges for nurses. Nurses are often caught between their personal beliefs and their professional duty to provide unbiased care to all patients.
Pro-Life: This perspective asserts that life begins at conception, viewing the unborn fetus as a person with the right to life, thus considering abortion morally wrong.
Pro-Choice: This viewpoint supports a woman’s right to control her own body, advocating that she should have the freedom to decide whether to continue a pregnancy.
This ethical dilemma is particularly challenging in nursing practice for several reasons:
- Personal Beliefs vs. Professional Duty: Nurses may feel conflicted when their personal beliefs about abortion clash with their duty to provide comprehensive care to patients seeking or having undergone an abortion.
- Patient Counseling: Nurses might struggle with providing information about all options, including abortion if doing so conflicts with their values.
- Emotional Stress: Caring for patients whose choices differ from the nurse’s personal beliefs can be emotionally taxing and stressful.
- Professional Standards: Nursing codes of ethics emphasize the importance of treating all patients with respect and fairness, regardless of the nurse’s personal beliefs.
To navigate these issues, nurses can focus on prioritizing the patient’s needs and rights. If a nurse has a strong objection to participating in an abortion, they should ensure the patient receives appropriate care by referring them to another qualified nurse. Maintaining open communication with patients and colleagues can help create an environment of respect and understanding.
End-of-Life Care Decisions
End-of-life care decisions represent some of the most profound challenges nurses face. The primary objective is to ensure patient comfort and honor their wishes, but ethical dilemmas can complicate this.
Nursing ethics emphasize a patient’s autonomy and their right to make informed choices. However, conflicts often arise when family members disagree with the patient’s preferences. In such cases, nurses find themselves navigating a delicate balance between respecting the patient’s wishes and acknowledging the family’s distress. Continuing aggressive treatments that offer minimal benefit and may cause further suffering is another ethical issue nurses must address.
For nurses, witnessing patient suffering is emotionally taxing. They may feel compelled to prioritize the patient’s comfort, even if it contradicts the physician’s plan. This situation can lead to moral distress, adding a significant emotional burden to their caregiving responsibilities.
Patient Confidentiality vs. Information Sharing
Balancing patient confidentiality with the need to share information is a crucial ethical dilemma in nursing. Patient confidentiality fosters trust, encouraging patients to be open and honest, which is essential for effective healthcare. However, certain situations necessitate sharing information, creating a complex ethical landscape for nurses.
For instance, when a nurse identifies a potentially contagious disease such as measles, reporting it to public health authorities may be necessary to prevent an outbreak. Similarly, if a nurse suspects elder abuse or domestic violence, they are legally and ethically obligated to report it to protect the vulnerable individuals involved.
Additionally, if a patient is a danger to themselves or others, breaking confidentiality may be required to ensure safety.
To navigate these ethical challenges, nurses should assess whether sharing information is necessary. They should explore alternative solutions that uphold confidentiality whenever possible. If disclosure is unavoidable, it is essential to share only the minimal amount of information required.
Transparency with the patient is also crucial; nurses should explain the reasons for sharing information and seek the patient’s consent when feasible.
Allocation of Limited Resources
From shortages in staffing to a lack of necessary equipment or medications, nurses regularly encounter the challenge of allocating limited resources efficiently. This often leads to intricate ethical dilemmas.
One of the most common constraints is understaffing, which forces nurses to spread themselves thin, impacting the quality of care they can provide. They must make tough decisions about prioritizing patient care and deciding who receives immediate attention when multiple patients are in critical need. This becomes especially challenging in emergencies, where nurses must triage patients, giving precedence to those with the most urgent conditions.
The emotional weight of these decisions can be significant, as it often involve making sacrifices about who receives timely care. Thankfully, many healthcare facilities offer established protocols and frameworks to assist nurses in making these difficult choices. These guidelines help ensure that resource allocation is done ethically and fairly, considering factors such as the severity of a patient’s condition, the likely benefit of treatment, and the overall scarcity of resources.
Refusal of Treatment by Patients
Refusal of treatment by patients presents a profound ethical dilemma for nurses. Picture a patient in a hospital bed, hooked up to various machines, telling the medical team, “I don’t want any more treatment.” This refusal can stem from fears of side effects, deeply held religious beliefs, or a wish for a natural death. When patients decline life-sustaining interventions like ventilators or dialysis, the ethical stakes are even higher, and nurses must ensure that patients fully comprehend the implications of their decisions.
This situation can take an emotional toll on nurses, leading to the following:
- Moral Distress: It can be heart-wrenching for nurses to watch patients refuse potentially life-saving treatments. Nurses may struggle with a sense of duty to protect their patients’ health while respecting their autonomy.
- Self-Care: To handle the emotional strain of such dilemmas, nurses need to prioritize their well-being. Utilizing hospital support systems and maintaining open communication with colleagues can be crucial in these moments.
For those juggling these challenges, our online nursing assignment help can lighten your academic load.
Balancing Patient Autonomy with Medical Advice
The nurse-patient relationship is intricate and founded on trust and mutual respect. Central to this relationship is the challenge of balancing patient autonomy with professional medical advice. Patients possess the right to make informed decisions about their healthcare, rooted in the ethical principle of respecting individuals’ autonomy. Meanwhile, nurses have to provide the best possible guidance based on their professional expertise. Achieving harmony between these two principles requires effective communication and a collaborative approach to decision-making.
Several obstacles can impede this balance. For example, patients may lack the medical background to grasp complex information fully. Nurses must, therefore, use clear, straightforward language and avoid overwhelming patients with medical terminology. Additionally, when a patient’s choice appears medically inadvisable, nurses should express their concerns, offering thorough explanations while ultimately honoring the patient’s right to decide. This approach ensures that both ethical principles are respected and upheld.
Cultural and Religious Conflicts
At the core of ethical dilemmas in nursing involving cultural and religious conflicts is often a gap in understanding. Individuals from diverse cultural backgrounds may hold different beliefs about the origins and treatments of illnesses. For example, some may attribute illness to spiritual factors, while others focus on environmental or lifestyle causes. Religious beliefs also play a significant role in a patient’s healthcare decisions, such as refusing specific medical interventions like blood transfusions due to faith-based prohibitions.
Recognizing that traditional healing practices often coexist with modern medical approaches is crucial. Although these practices might appear unconventional from a Western medical standpoint, dismissing them can lead to patient alienation and impact their recovery negatively. Embracing and respecting these traditions, even when they differ from conventional methods, helps build a trusting and collaborative relationship with patients.
Culturally competent nurses are better equipped to deliver effective care. By understanding and respecting the diverse cultural and religious backgrounds of their patients, nurses can foster empathy, trust, and improved healthcare outcomes.
Use of Restraints and Seclusion
Restraints and seclusion are sometimes necessary in nursing to protect patients or others from harm. However, their use raises significant ethical concerns and should be considered a last resort.
Ethical Concerns:
- Violation of Autonomy: Restraining a patient restricts their freedom of movement, which is a fundamental human right. Seclusion can also feel punitive and isolating, causing emotional distress.
- Risk of Injury: The use of restraints can lead to physical injuries, such as bruises or pressure sores. The psychological impact of being restrained can also be deeply traumatic for some patients.
The goal should be to minimize or eliminate the need for restraints and seclusion. This can be achieved by creating a safe and soothing environment to reduce the likelihood of self-harm or aggressive behavior. Strategies include removing potential hazards and using sensory tools to provide comfort. Employing de-escalation techniques, such as active listening, speaking calmly, and providing a quiet space, can effectively manage a patient’s agitation without resorting to restraints.
Handling Unethical Behavior by Colleagues
Dealing with unethical behavior by colleagues in nursing can place nurses in a challenging position. Observing actions that violate nursing ethics creates a dilemma—whether to report the behavior or remain silent.
The foremost concern should always be patient safety. Unethical conduct by a colleague can jeopardize patient well-being, making it crucial to address the issue. Reporting such behavior helps foster a culture of safety within the healthcare environment, demonstrating a commitment to ethical practices and zero tolerance for misconduct.
Despite the importance of speaking up, nurses often fear retaliation from the colleagues involved or even from superiors, who may prefer to avoid the conflict. The strong sense of unity within nursing teams can also complicate the decision to report a colleague. However, failing to address unethical behavior due to misplaced loyalty can lead to harmful outcomes.
When witnessing unethical behavior, it is essential to document all details—what occurred, when it happened, and any witnesses present. This documentation can be vital if a formal report is necessary. Utilizing anonymous reporting systems can also be an option for those concerned about potential retaliation.
Disclosing Medical Errors
Mistakes can occur even in the most carefully managed healthcare settings, presenting nurses with the ethical challenge of whether to disclose the error to patients and their families.
The Importance of Transparency:
- Patient Rights: Patients deserve to be fully informed about their care, including any errors that occur.
- Improving Healthcare: Transparent disclosure helps identify and correct systemic problems in healthcare.
- Trust Building: Although difficult, honesty about errors strengthens trust over time.
Disclosing medical errors can be emotionally challenging for both nurses and patients. Nurses may fear repercussions, while patients might feel anger, fear, or a breach of trust. Nonetheless, transparency in disclosing medical errors is the ethical and responsible choice.
How to Deal With Ethical Dilemmas in Nursing
Navigating ethical dilemmas in nursing requires a structured approach. Here are some strategies from our nursing writing service to help you handle these challenging situations effectively:
Step | Description | Details |
Identify the Dilemma ⚖️ | Recognize that you are facing an ethical dilemma. | This may involve conflicting ethical principles, unclear courses of action, or emotional discomfort. |
Collect Information 📋 | Gather all relevant information about the situation. | Consider the patient’s medical condition, their wishes, potential outcomes, and applicable policies. |
Evaluate Your Options 🤔 | Consider various possible solutions. | Weigh the ethical principles, the patient’s best interests, and the potential risks and benefits of each option. |
Seek Advice 🗣️ | Consult with others to gain different perspectives. | Engage with experienced colleagues, healthcare professionals, and ethics committees. |
Document Your Process 📝 | Keep thorough records of your decision-making process. | Include details of the dilemma, information collected, options considered, and the final decision made. |
Reflect on the Outcome 💭 | Reflect on the experience after the situation is resolved. | Think about what you learned, how you might handle similar situations in the future, and any areas for improvement. |
Ethical Dilemmas in Nursing Examples
Nurses are committed to providing high-quality care, respecting patient autonomy, and acting in their patients’ best interests. However, real-world scenarios often present complex ethical dilemmas. Here are a few examples:
Scenario 1: The Ventilator Shortage
In a busy intensive care unit, two patients urgently need a ventilator due to severe respiratory distress. Unfortunately, there is only one ventilator available.
Solution:
Most hospitals have triage protocols to prioritize patients based on the severity of their condition and the likelihood of recovery. Nurses must follow these guidelines, communicate openly with both patients’ families, and advocate for more resources to prevent future shortages.
Scenario 2: Patient Refusal of Treatment
A competent adult patient with a terminal illness decides to refuse life-extending treatment, such as chemotherapy, despite their family’s objections.
Solution:
The nurse must respect the patient’s autonomy, ensuring they are fully informed about the consequences of their decision. Providing support and information to the family while respecting the patient’s wishes is essential.
Scenario 3: Cultural and Religious Beliefs
A patient who is a devout Jehovah’s Witness requires a blood transfusion after an accident but refuses due to their religious beliefs.
Solution:
The nurse should respect the patient’s beliefs and explore alternative treatments, such as bloodless surgery techniques. Collaboration with a cultural mediator or religious leader can help find a mutually acceptable solution.
Scenario 4: Medication Error Disclosure
A nurse accidentally administers the wrong medication to a patient. Although the patient experiences no immediate harm, the nurse is concerned about potential repercussions.
Solution:
Transparency is crucial. The nurse should report the error according to hospital protocols, inform the patient and their doctor, and focus on preventing further harm. Support from colleagues and supervisors can help manage the stress of disclosure.
Final Remarks
Ethical dilemmas in nursing are an inevitable part of the profession, presenting significant challenges that require careful consideration and compassionate decision-making. By understanding common ethical issues, such as resource allocation, patient autonomy, and cultural conflicts, nurses can better prepare to handle these situations with integrity and professionalism. Employing strategies like gathering comprehensive information, seeking consultation, and reflecting on experiences can aid in navigating these complex scenarios. Ultimately, maintaining a commitment to ethical principles not only enhances patient care but also reinforces the trust and respect essential to the nursing profession.

Dreading that Looming Deadline for Your Nursing Paper?
Sleep soundly! Our team of expert writers is here to help.
FAQs
What are some ethical dilemmas in nursing?
Ethical dilemmas in nursing often involve conflicts between different values and principles. Common dilemmas include deciding between pro-life and pro-choice in reproductive care, managing end-of-life care decisions, balancing patient confidentiality with the need to share information for their benefit, and allocating limited medical resources fairly.
What are some examples of ethical dilemmas that might cause moral distress?
Examples of ethical dilemmas that might cause moral distress include situations where a nurse must respect a patient’s refusal of life-saving treatment, navigate cultural or religious beliefs that conflict with medical advice, and decide whether to disclose a medical error that could have serious consequences. These situations often leave nurses feeling torn between their professional duties and their ethics.
What are the 4 types of ethical dilemmas?
The four types of ethical dilemmas typically encountered in nursing are:
- Autonomy vs. Beneficence: Respecting a patient’s personal choices versus acting in their best health interest.
- Truth-telling vs. Non-maleficence: Being honest with patients versus avoiding harm, which can sometimes conflict.
- Justice vs. Resource Allocation: Fairly distributing limited resources while ensuring patients receive adequate care.
- Professional Integrity vs. Ethical Responsibilities: Upholding professional standards versus the ethical duty to report misconduct or errors.
What is an example of an ethical dilemma?
An example of an ethical dilemma in nursing is when a patient with a terminal illness refuses further treatment that could prolong their life. The nurse must respect the patient’s autonomy and right to refuse treatment, even if they believe that continuing treatment is in the patient’s best interest. Balancing respect for the patient’s wishes with the desire to provide life-saving care can be challenging and emotionally taxing.
Sources
Duquesne University. Ethical issues in Nursing: Explanations & Solutions. https://onlinenursing.duq.edu/blog/ethical-issues-in-nursing/
Nurse Org. 10 Examples of Ethical Dilemmas in Nursing. https://nurse.org/education/ethical-dilemmas-nursing/

